Page 2 - hypertension_newsletter7
P. 2
REFLECTIONS
Hypertension
Hypertension Global Newsletter #7 2024
GUIDELINES Hypertension
2024 ESC guidelines for the management of elevated blood pressure and
hypertension.
McEvoy JW, et al. Eur Heart J. 2024 Aug 30:ehae178. doi: 10.1093/eurheartj/ehae178. Online ahead of print.
The European Society of Cardiology (ESC) recently presented new guidelines for managing elevated BP and hypertension. These
guidelines use the most robust contemporary evidence and aim to provide a simplified classification of BP and management of
individuals with elevated BP and hypertension.
The new guidelines continue to define hypertension as a SBP of ≥140 mmHg and DBP ≥90 mmHg, but now also include a
new category of elevated BP, which is defined as SBP of 120–139 mmHg or a DBP or 70–89 mmHg, with a strongly related
recommendation to perform a CV risk assessment to guide treatment, especially in those with BP of at least 130/80 mmHg.
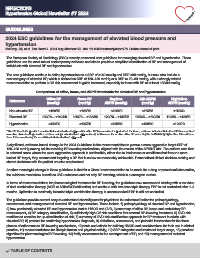
Comparison of office, home, and ABPM thresholds for elevated BP and hypertension
Office BP Home BP Daytime 24h ABPM Night-time
Reference (mmHg) a (mmHg) ABPM (mmHg) (mmHg) ABPM (mmHg)
Non-elevated BP <120/70 <120/70 <120/70 <115/65 <110/60
Elevated BP 120/70 – <140/90 120/70 – <135/85 120/70 – <135/85 115/65 – <130/80 110/60 – <120/70
Hypertension ≥140/90 ≥135/85 ≥135/85 ≥130/80 ≥120/70
a The BP thresholds provided assume that a standardized approach to office BP measurement is performed. However, evidence indicates that office BP measurement
in routine clinical settings is often not done using a standardized approach and, in this case, the routine office BP value may be 5–10 mmHg higher than it would have
been if measured using the recommended standardized approach
A significant, evidence-based change in the 2024 Guidelines is the recommendation to pursue a more aggressive target SBP of
120–129 mmHg among adults receiving BP-lowering medications, aligned with the results of the SPRINT trial. The authors note that
in selected cases where the more aggressive approach is not feasible, either due to intolerance or conditions that favour a more
lenient BP target, they recommend targeting a BP that is as low as reasonably achievable. Personalised clinical decision-making and
shared decisions with the patient are also emphasised.
Another meaningful change in these guidelines is that for a Class I recommendation to be made for a drug or procedural intervention,
the evidence must show benefit on CVD outcomes and not only BP lowering, which is a surrogate marker.
In terms of recommendations for pharmacological treatment for BP lowering, the guidelines now recommend starting with a low dose
of dual combination therapy (ACEi or ARBs/CCBs/diuretics) and continue with low-dose triple therapy if BP is not controlled after 1–3
months. Uptitration to maximally tolerated triple combination therapy is recommended if BP is still not controlled.
The guidelines provide several easy-to-understand charts/figures for physicians to understand better the pathophysiology,
assessment, and management of elevated BP and hypertension. These include 1) pathophysiology of elevated BP and hypertension,
2) how persistently elevated BP and hypertension lead to HMOD and CVD, 3) summary of office BP, home and ambulatory BP
measurement, 4) BP category classification, 5) sufficiently high CV risk conditions that warrant BP-lowering treatment, 6) CVD risk
modifiers to consider for up-classification of risk, 7) summary of CVD risk-stratification approach for BP treatment in adults with
elevated BP, 8) protocol for confirming hypertension diagnosis, 9) definitions, assessment, and potential intervention for the three
phases of adherence to BP-lowering medications, 10) tests and criteria for defining HMOD and considerations for their use in clinical
practice, 11) recommendations for lifestyle factors and physical activity, 12) SBP categories and treatment target range, 13) practical
algorithm for pharmacological BP lowering, 14) frailty assessment in the management of BP, and 15) management of resistant
hypertension.
TABLE OF CONTENTS